- ✓Semaglutide & tirzepatide injections prescribed online by U.S. doctors
- ✓Convenient telehealth care with ongoing support
- ✓Simple online process—get evaluated and treated from home
How GLP-1 Changes Everything When Food Feels Like an Addiction
Why cravings, food noise, and constant hunger aren’t a willpower problem — and how GLP-1 support helps restore balance.

You tell yourself you’re not even that hungry — but the pull is still there. The cravings come out of nowhere. The urge to snack, graze, or reach for something comforting feels automatic. Sometimes it feels less like a choice and more like something your body demands.
You try to resist. You try to “be good.” You promise yourself this time will be different. But the thoughts keep circling. Food becomes louder than everything else.
And eventually, frustration turns into confusion. Why does food have this kind of control? Why does willpower seem to disappear the moment stress, fatigue, or emotion kicks in?
Here’s the truth most people never hear: when food feels addictive, it’s rarely a lack of discipline. It’s usually a biological loop that’s been thrown out of balance.
For many people — especially those dealing with chronic inflammation, autoimmune conditions, hormonal disruption, or long-term metabolic stress — cravings don’t operate the same way. The body’s signaling system is altered. Hunger cues misfire. Satisfaction is delayed or missing entirely.
And when that happens, food stops feeling like nourishment and starts behaving more like a drug.
- Cravings feel automatic — not “you being weak.”
- Stress and fatigue can amplify food noise fast.
- When fullness signals are delayed, you keep searching for “enough.”
Why Food Cravings Can Feel Impossible to Control
When the body is under constant stress, everything changes — especially how hunger and reward are regulated.
Inflammation interferes with the hormones that control appetite and fullness. Blood sugar becomes harder to stabilize. Stress hormones stay elevated. The brain begins searching for quick sources of comfort and energy.
Highly processed foods are engineered to deliver exactly that. They light up reward centers, release dopamine, and create a short-lived sense of relief — especially when energy is low or emotions are high.
But the relief never lasts.
Blood sugar spikes, then crashes. Hunger returns quickly. Cravings grow stronger. And over time, the brain begins to associate food not with nourishment, but with emotional regulation.
That’s when eating stops feeling like a choice.
- Spike → crash cycles can make hunger return faster.
- Dopamine-driven relief trains the brain to “want more.”
- Restriction can backfire when the body senses danger.
For people dealing with chronic inflammation or metabolic dysfunction, this cycle becomes even harder to break. Appetite hormones lose their rhythm. Fullness signals arrive late or not at all. The body stays in a constant state of “need.”
This is why advice like “just eat less” feels insulting to so many people.
The issue isn’t willpower. It’s that the system controlling hunger, satisfaction, and impulse is out of sync.
When Food Starts Running the Show
Once this cycle sets in, eating becomes mentally exhausting.
You think about food more than you want to. You feel guilty after eating. You promise yourself tomorrow will be different.
But the more you restrict, the louder the cravings become.
This isn’t because you’re weak. It’s because your body interprets restriction as danger.
And when survival mode is activated, cravings feel urgent, emotional, and overwhelming.
Where GLP-1 Changes the Story
GLP-1 therapy works differently than traditional approaches to appetite or weight control. It doesn’t rely on restriction, guilt, or discipline. It restores regulation.
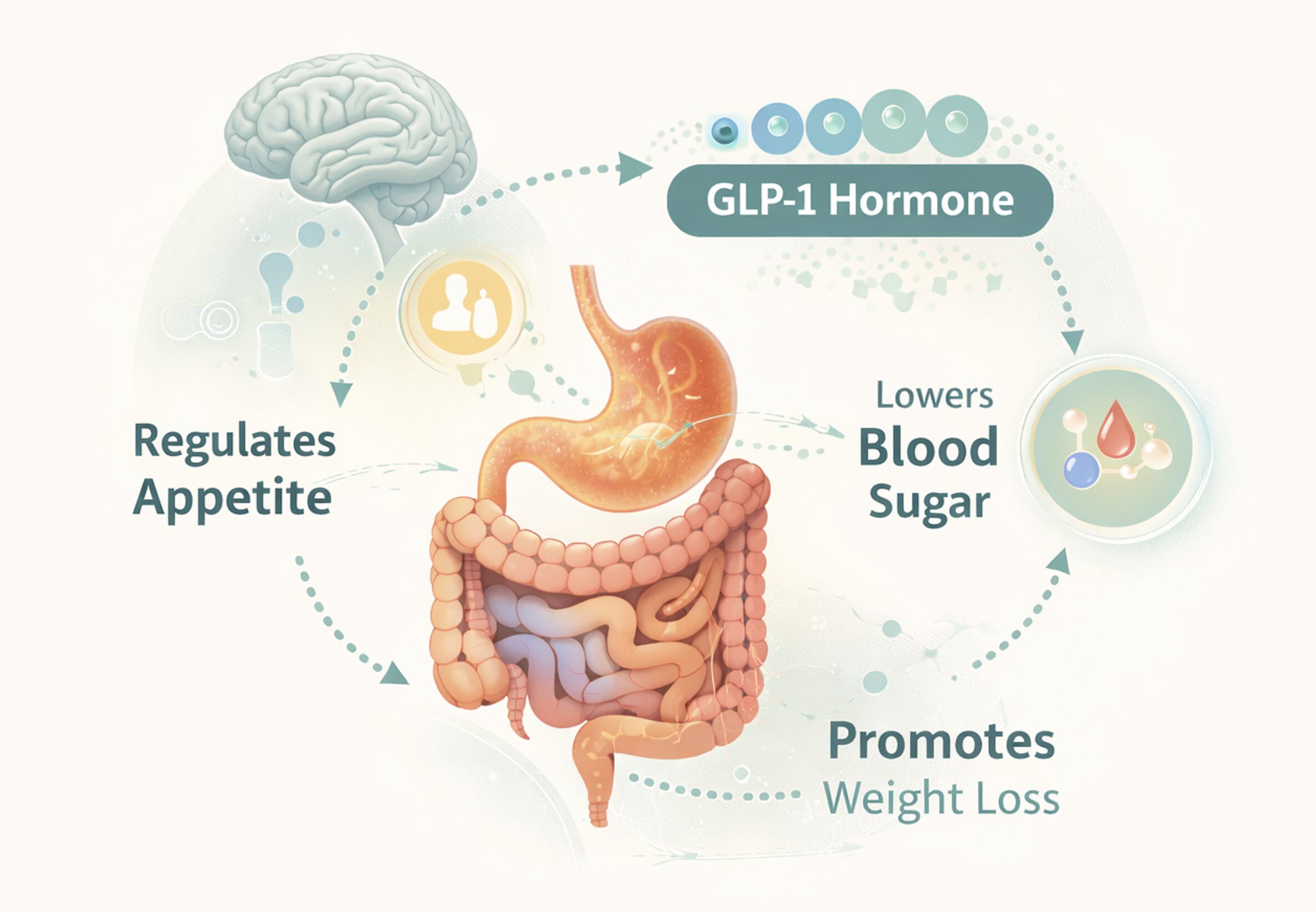
GLP-1 is a hormone your body already produces. It helps manage appetite, slow digestion, stabilize blood sugar, and signal fullness to the brain.
- Helps quiet “food noise” by improving fullness signaling.
- Supports steadier blood sugar — fewer crashes, fewer urgent cravings.
- Slows digestion so meals feel more satisfying, longer.
When this system works properly, eating feels normal. Cravings quiet down. Food stops dominating your thoughts.
When GLP-1 signaling is impaired, hunger becomes louder and satisfaction fades. GLP-1 support options help correct that imbalance.
Many people describe the change as subtle but powerful. They’re not forcing themselves to eat less — they just don’t feel driven to eat the same way.
Why This Matters for Chronic Inflammation
GLP-1 doesn’t treat autoimmune disease directly, but it reduces metabolic strain — one of the biggest obstacles to healing.
- Less metabolic strain can mean more “good energy” days.
- Steadier blood sugar often feels like fewer highs-and-lows.
- Reduced joint stress can make movement feel more doable.
As blood sugar stabilizes, inflammation often becomes easier to manage. Energy improves. Brain fog lifts. Joint stress decreases.
For many people, weight loss becomes a side effect — not the goal.
Why More People Are Turning to GLP-1
For years, people were told to try harder. Eat less. Be more disciplined.
Now we know better.
Cravings and weight resistance are often biological, not personal failures. GLP-1 works with the body instead of against it.
- It’s not about “perfect dieting” — it’s about calmer signals.
- It’s not about shame — it’s about regulation and support.
- It’s not about white-knuckling — it’s about feeling normal around food again.
This isn’t about the scale. It’s about feeling calm around food again. Feeling capable. Feeling in control.
Choosing the Right GLP-1 Option Matters
Not all GLP-1 programs are the same. Some focus on cost. Others prioritize support or medical oversight.
The right choice depends on your health history, your goals, and how much guidance you want.
- Want structure and guidance? Look for stronger coaching/support.
- Want simplicity? Look for streamlined onboarding and refill flow.
- Want confidence? Compare reputable GLP-1 providers side-by-side.
Below, we’ll break down the top GLP-1 provider options so you can compare your options and choose what fits you best.
- ✓Semaglutide & tirzepatide options with clinician guidance
- ✓Streamlined onboarding and easy at-home delivery
- ✓Great balance of support + affordability
- ✓GLP-1 support with clinician oversight
- ✓Designed for a smooth online experience
- ✓Solid choice for consistent care and convenience
- ✓Online access to clinician-guided options
- ✓Clear process with ongoing support
- ✓Strong overall performance across key criteria
- ✓Well-rounded program option
- ✓Good choice for those wanting a straightforward experience
- ✓Competitive ratings across the board
- ✓Semaglutide & tirzepatide injections prescribed online by U.S. doctors
- ✓Convenient telehealth care with clinician support
- ✓Easy evaluation + delivery—get started from home
Frequently Asked Questions
How do prescription weight loss medications actually work?
Most prescription weight loss medications work by targeting your body's hunger signals and metabolism. GLP-1 medications, for example, mimic a natural hormone that tells your brain you're full, which helps reduce cravings and portion sizes. They also slow down how quickly your stomach empties, so you feel satisfied longer after eating. Some medications affect how your body processes fat and sugar, while others work on neurotransmitters that control appetite. The key thing to remember is that these medications work best alongside healthy eating and regular physical activity—they're designed to support your efforts, not replace them.
Am I a good candidate for weight loss medication?
Typically, healthcare providers consider weight loss medications for adults with a BMI of 30 or higher, or a BMI of 27 or higher if you have weight-related health concerns like high blood pressure, sleep apnea, or prediabetes. That said, BMI isn't the whole story—your doctor will look at your complete health picture, including your weight loss history, current medications, and any existing medical conditions. The best way to know if you're a candidate is to have an honest conversation with your healthcare provider about your weight loss goals and challenges. They can help determine if medication is a safe and appropriate option for your specific situation.
What side effects should I expect?
The most common side effects are digestive-related—things like nausea, occasional vomiting, diarrhea, or constipation. These usually show up when you first start treatment or increase your dose, and they typically get better as your body adjusts over a few weeks. Some people also experience headaches, fatigue, or dizziness. For injectable medications, you might have some tenderness at the injection site. While serious side effects are rare, they can include gallbladder issues, pancreatitis, or changes in heart rate. Your doctor will monitor you closely, especially in the beginning. Most people find that starting with a lower dose and gradually increasing it helps minimize side effects.
How long does it take to see results?
Most people start noticing changes within the first month—reduced hunger, better control over cravings, and the scale starting to move in the right direction. Significant weight loss typically happens over 3 to 6 months, with many people continuing to see progress for up to a year or more. The pace varies from person to person based on your starting weight, metabolism, activity level, and how consistently you follow your treatment plan. It's important to set realistic expectations: safe, sustainable weight loss is gradual. Think of it as a marathon, not a sprint. The people who see the best long-term results are those who combine medication with lifestyle changes they can maintain over time.
Will my insurance cover weight loss medication?
Insurance coverage for weight loss medications is honestly all over the map. Some plans cover them, especially if you have related health conditions like type 2 diabetes or cardiovascular disease. Others don't cover them at all, viewing them as elective or cosmetic. Medications approved specifically for diabetes (like Ozempic®) may have better coverage than those approved purely for weight management (like Wegovy®), even though they contain the same active ingredient. Your best bet is to call your insurance company directly and ask about coverage for the specific medication your doctor recommends. Also ask about prior authorization requirements and copay amounts. If insurance won't cover it, many telehealth companies and clinics offer more affordable self-pay options or payment plans.
What are the main differences between Ozempic®, Wegovy®, and Mounjaro®?
Ozempic® and Wegovy® both contain semaglutide, but Wegovy® comes in higher doses and is FDA-approved specifically for weight loss, while Ozempic® is approved for type 2 diabetes (though weight loss is a common side effect). Mounjaro® contains tirzepatide, which works on two hormone pathways instead of one, potentially leading to more weight loss for some people. It's currently approved for diabetes, with weight loss approval pending. The main practical differences are dosing schedules, maximum doses, insurance coverage, and how your body responds to each. Some people do better on one than another due to side effects or effectiveness. Your healthcare provider can help you figure out which option aligns best with your health needs and goals.
Do I need to take this medication forever?
This is a great question that doesn't have a one-size-fits-all answer. Clinical studies show that many people regain weight after stopping these medications, which suggests they may need to be taken long-term to maintain results. Think of it like managing blood pressure or cholesterol—some conditions require ongoing treatment. That said, every situation is different. Some people successfully transition off medication after establishing solid healthy habits, while others find they need to stay on it to maintain their progress. The decision should be made with your doctor based on your weight loss goals, overall health, and how your body responds. The key is having a realistic plan for maintaining your results, whether that includes medication or not.
Can I drink alcohol while taking weight loss medication?
Moderate alcohol consumption is generally considered safe while taking most weight loss medications, but there are some important considerations. Alcohol can worsen side effects like nausea and dizziness, especially when you're first starting treatment. It also adds empty calories that can slow your weight loss progress. Some people find that medications like GLP-1s naturally reduce their desire to drink alcohol. If you have a history of pancreatitis or gallbladder issues, your doctor might recommend limiting or avoiding alcohol altogether. The bottom line: occasional, moderate drinking is usually okay, but check with your healthcare provider about your specific situation. And remember, part of successful weight loss often involves rethinking habits—including how alcohol fits into your lifestyle.
Are compounded versions of these medications safe?
Compounded medications can be a legitimate option when manufactured by licensed, reputable compounding pharmacies that follow strict quality standards. However, they're not FDA-approved, which means they haven't gone through the same rigorous testing as brand-name medications. The FDA has issued warnings about counterfeit and improperly compounded versions circulating online. If you're considering a compounded option due to cost or availability, make sure it comes from a pharmacy that's registered with your state board and ideally accredited by organizations like PCAB. Never buy medication from random websites or social media ads. Your healthcare provider can help you weigh the risks and benefits of compounded versus brand-name options and ensure you're getting medication from a trustworthy source.
What happens if I miss a dose?
Don't panic if you miss a dose—it happens! For weekly injections like semaglutide or tirzepatide, if you remember within 5 days of your scheduled dose, take it as soon as you remember, then continue your regular weekly schedule. If it's been more than 5 days, skip that dose and take your next one on your regular day. Never double up on doses to make up for a missed one. For daily medications, take the missed dose as soon as you remember unless it's almost time for your next scheduled dose. Missing an occasional dose won't derail your progress, but try to stay consistent for the best results. Set phone reminders or use a medication tracking app if you tend to forget. If you're frequently missing doses, talk to your doctor about strategies to help you stay on track.
Will I lose muscle mass along with fat?
Whenever you lose weight—whether through diet alone or with medication—you’ll typically lose some muscle along with fat. The ratio depends on how you approach weight loss. To preserve as much muscle as possible while on weight loss medication, focus on eating enough protein (aim for 0.7–1 gram per pound of body weight), incorporate resistance training at least 2–3 times per week, and avoid losing weight too rapidly. Some studies suggest that GLP-1 medications may cause more muscle loss than traditional diet and exercise alone, which makes strength training even more important. Your healthcare provider or a registered dietitian can help you create a plan that maximizes fat loss while protecting your muscle mass. Remember, the goal isn’t just to weigh less—it’s to be healthier and stronger.

The information on this website is provided for general educational purposes only and is not medical advice. Always consult a qualified healthcare professional before starting, stopping, or changing any medication or treatment. Individual results may vary.
© Functional Living Guide.
All rights reserved.